BMC Women's Health volume 23, Article number: 286 (2023 ) Cite this article
Associations of luteinizing hormone (LH) with androgens during the menopausal transition and associations between follicle-stimulating hormone (FSH) levels and various diseases related to reproductive hormones in postmenopause have received much attention. LH and FSH are also known to be associated with activities of enzymes related to reproductive hormones. We examined the associations of LH and FSH with androgens and estrogens in each stage of the menopausal transition according to a classification from menopausal transition to postmenopause. Urine During Menopause
This study was a cross-sectional design. We basically used the Stage of Reproductive Aging Workshop (STRAW) + 10. We divided the 173 subjects into 6 groups according to menstrual regularity and follicle-stimulating hormone level: mid reproductive stage (Group A), late reproductive stage (Group B), early menopausal transition (Group C), late menopausal transition (Group D), very early postmenopause (Group E) and early postmenopause (Group F). Levels of LH, FSH, dehydroepiandrosterone sulfate (DHEAS), estradiol, estrone, testosterone (T), free T, androstenedione and androstenediol were measured.
In Group A, LH showed significant positive correlations with androstenedione and estrone. In Group D, LH was positively associated with T and free T and was negatively associated with estradiol. In Groups B, C, D and F, LH showed significant positive correlations with FSH, and there was a tendency for an association between LH and FSH in Group E. FSH was associated with estradiol but not with estrone in Groups C and D.
The associations of LH and FSH with reproductive hormones are different depending on the stage of the menopausal transition.
Trial registration number 2356-1; Date of registration: 18/02/2018, retrospectively registered.
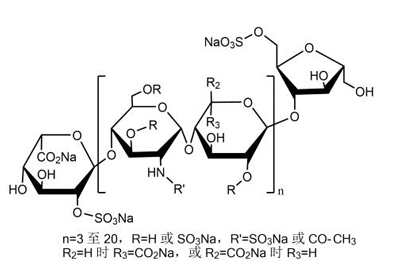
During the menopausal transition, the production of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) in the pituitary increases to compensate for the declining estradiol levels due to a decrease in ovarian function. Based on changes in FSH trajectory accelerations and decelerations and rates of change, four menopausal transition stages bounding the final menstrual period and eight epochs in chronological aging from ages of 28 to 60 years have been defined [1]. Also, in women aged 42–52 years, three FSH trajectories over the menopausal transition have been identified [2]. Previous studies have shown that FSH receptors are distributed in various tissues including the bone [3, 4], liver [5] and vessels [6] as well as the ovary. It has been shown that FSH has extragonadal actions and that FSH levels are associated with various diseases and with metabolism in postmenopause [7, 8]. On the other hand, LH receptors are also distributed in not only the ovary but also the adrenal gland [9], brain [10], skin [11] and bladder [12]. It has been reported that an LH level of less than 41 U/L showed a positive correlation with dehydroepiandrosterone sulfate (DHEAS) level in postmenopausal women but not in women during the menopausal transition [13], suggesting that DHEAS production from the adrenal gland may be stimulated by highly elevated LH levels [13]. Although much attention has been focused on the delta-4 steroidogenic pathway that produces cortisol, androstendione and testosterone, longitudinal studies have suggested that the delta-5 steroidogenic pathway that produces DHEA as shown in Fig. 1, DHEAS and androstenediol may play a more important role in women’s healthy aging [14, 15]. It has been reported that gonadotropins such as LH and FSH change the activities of enzymes, including cytochrome P450 (CYP) 17 A, 3β-hydroxysteroid dehydrogenase (HSD) and 17β-HSD, that act in the delta-4 and delta-5 steroidogenic pathways [16,17,18,19]. During the menopausal transition, increases in LH and FSH levels change the activities of enzymes and might be associated with changes in the levels of reproductive hormones.
17OH pregnenolone: 17-hydroxyprogesterone, CYP17A1: cytochrome P450 17A1, 17βHSD: 17β-hydroxysteroid dehydrogenases, 3βHSD: 3β-hydroxysteroid dehydrogenase.
In 2012, the Stage of Reproductive Aging Workshop (STRAW) + 10 staging system was revised. The revised staging system improves the comparability of studies of midlife women and is widely considered as the gold standard for characterizing reproductive aging through menopause [20]. Based on the STRAW staging system, we found associations of androstenediol levels related to the delta-5 steroidogenic pathway with estrogen and androgen in women during the menopausal transition in a previous study by using liquid chromatography mass spectrometry (LC-MS/MS) with high sensitivity and high specificity [21]. Associations of LH with androgens during the menopausal transition have been shown, but there has been no report on the associations between FSH and androgens including androstenediol. The associations of LH and FSH with reproductive hormones related to the adrenal gland may differ according to each stage in the STRAW classification. To our knowledge, information on the associations of gonadotropins, including LH and FSH, with androgens and estrogens in premenopausal women, women during the menopausal transition and postmenopausal women is scarce. Thus, we aim to elucidate the associations of LH and FSH levels with reproductive hormone levels in premenopausal women, women in the menopausal transition and postmenopausal women.
We recruited 173 Japanese women for this cross-sectional study from the outpatient clinic of the Department of Obstetrics and Gynecology in Tokushima University Hospital. These women visited a specialized health care outpatient clinic for consultation and for management and treatment of various conditions including decrease in bone mineral density, dyslipidemia and menopausal symptoms. Women who had received hormone therapy in the past year were excluded. At the time of the visit to the outpatient clinic, we obtained information on menstrual frequency and flow or years since the final menstrual period (FMP) and we measured FSH level and determined the stage of menopausal transition. Based on the STRAW staging system [20], we divided the subjects into 6 stages by menstrual regularity and FSH level: (1) women with a regular menstrual cycle (25–35 days per cycle) and normal FSH level (mid reproductive stage, Group A, n = 21), (2) women with a regular menstrual cycle and elevated FSH level (> 10 mIU/ml) (late reproductive stage, Group B, n = 22), (3) women with an irregular menstrual cycle and elevated FSH level (> 10 mIU/ml) (early menopausal transition, Group C, n = 23), (4) women who had an irregular menstrual cycle in which the interval of amenorrhea was more than 2 months and who had elevated FSH level (late menopausal transition, Group D, n = 35), (5) women for whom less than 1 year had passed since menopause (very early postmenopause, Group E, n = 30), and (6) women for whom more than 1 year and less than 5 years had passed since menopause (early postmenopause, Group F, n = 42). Informed consent for participation in this study was obtained from each woman. The Ethics Committee of Tokushima University Hospital approved the study.
Blood in women with menstruation was drawn from 9:00 to 12:00 during a period of 3–7 days after the commencement of menstruation. Blood samples for measurements were obtained by venipuncture and drawn into tubes. They were frozen at -40℃ until used for analysis. Levels of LH, FSH, estradiol and testosterone (T) were measured by a chemiluminescent immunoassay. DHEAS level was measured by a chemiluminescent enzyme immunoassay. Levels of androstenedione and free T were measured by a radioimmunoassay. The intra- and inter-assay coefficients (CVs) for DHEAS, T, free T, estradiol, androstenedione, LH and FSH were less than 10%. Serum androstenediol and estrone concentrations were measured by using LC-MS/MS, and the measurements were described in our previous report (21). The intra- and inter-assay CVs for androstenedione measurements were 2.3–2.9% and 4.4–6.3%, respectively. The intra- and inter-assay CVs for estrone measurements were 2.0-2.3% and 3.0-3.2%, respectively. The sensitivity of the assay was 0.01 ng/ml for androstenediol and estrone.
All statistical analyses were performed by using SPSS statics version 20.0 (IBM, Armonk, New York). Data are presented as medians with 25th and 75th ranges and LH/FSH ratio is shown as a mean. The Kruskal-Wallis rank test was used to compare differences between different menopausal stages, and Bonferroni adjustment was used for a multiple comparison test. Correlations between variables were assessed by Spearman’s rank correlation analysis.
Background characteristics of the subjects are shown in Table 1. Median body mass index (BMI) ranged from 20.1 to 22.5 kg/m2, and there was no significant difference in BMI among the groups. BMI in one woman was more than 30.0 kg/m2 (Table 1). None of the study subjects had dyslipidaemia or diabetes, or hypertension requiring any medication.
Levels of LH and FSH in premenopausal women, women during the menopausal transition and postmenopausal women are shown in Fig. 1. Both LH and FSH levels were significantly high in Groups D, E and F compared to those in Group A. In addition, LH level tended to be high in Group C compared to that in Group A (p = 0.062).
FSH level continued to high after Group D, but LH level reached a plateau at Group E (Fig. 1A and B). There was no significant difference in the LH/FSH ratio among the 6 groups (Table 1).
The box indicates values from the 25th percentile to the 75th percentile. The vertical line in the box indicates the median and the cross mark indicates the mean. Vertical lines represent minimum and maximum values. * p < 0.05 vs. Group A. # p = 0.06 vs. Group A.
Group A: mid reproductive stage, Group B: late reproductive stage, Group C: early menopausal transition, Group D: late menopausal transition, Group E: very early post menopause, Group F: early postmenopause.
As can be seen in Table 2, in Group A, LH level showed significant and positive correlations with levels of androstenedione and estrone (r = 0.747, p = 0.003; r = 0.782, p = 0.038). In Group D, LH level was positively associated with levels of T and free T (r = 0.356, p = 0.036 and r = 0.414, p = 0.041, respectively) and was negatively associated with estradiol level (r=-0.484, p = 0.003). Positive associations between LH and FSH were found in Groups B, C, D and F (r = 0.713, p < 0.001; r = 0.776, p < 0.001; r = 0.692, p < 0.001; r = 0.688, p < 0.001), and a tendency for a positive correlation between LH and FSH was found in Group E (r = 0.358, p = 0.052) (Table 2). Significant correlations are also shown as scatterplot figures (Fig. 2A).
LH and FSH levels in premenopausal women, women during the menopausal transition and postmenopausal women
In Groups C and D, FSH level showed a significant and negative association with estradiol level (r=-0.432, p = 0.039 and r=-0.720, p < 0.001, respectively) but not with estrone level. FSH level was not associated with testosterone, DHEAS, androstenediol or androstenedione (Table 3). Significant correlations are also shown as scatterplot figures (Fig. 2B).
Significant correlations between LH and reproductive hormones are shown in Fig. 2A. In Group D, LH level was positively associated with levels of T and free T and was negatively associated with estradiol level. Significant correlations between FSH and reproductive hormones are shown in Fig. 2B. In Groups C and D, FSH level showed a significant and negative association with estradiol level.
In the present study, we found that the associations of LH and FSH with reproductive hormones differ according to stages of the menopausal transition.
Women in Group A had a normal range of FSH levels. However, the ages of women in Group A ranged from 41.6 to 46.5 years and gradually approached the age for menopause. The fact that the delta-4 pathway for synthesis of androstenedione and estrone acts well along with actions of 17β-HSD and 3β-HSD in women in that age range is thought to be the reason for the significant correlations of LH level with estrone and androstenedione levels in Group A. In women in Group A, the delta-4 pathway in the ovary may have been maintained due to a balance between LH and FSH.
In Group B, in which ovarian function had begun to decrease, there was no significant association of LH level with androstenedione or estrone level. Through an increase in FSH level, a relationship in which the balance between LH and FSH was maintained in Group A was considered to attenuate, and the shift might be beginning toward the delta-5 pathway. In addition, stimulation of DHEAS production in the ovary by augmentation of CYP17A1 activity due to an increase in LH may be the reason for the disappearance of correlations of LH with androstenedione and estrone. A correlation between LH and FSH was found with increasing FSH level.
In several studies, fibrosis in the stroma was observed in the ovary and associations between LH and androgens were found in women approaching menopause. Reproductive age-associated fibrosis was found in the stroma of ovaries in mice and humans [22, 23]. Matt et al. reported that alterations in hypothalamic-pituitary function such as a prolonged interpulse interval of LH and increased LH pulse width were found in middle-aged women with a mean age of 42.6 years [24]. A tripartile relationship among increase in LH, increase in androgens and fibrosis in the stroma in the ovary was also found in women with polycystic ovary syndrome (PCOS) [25]. Wickenheisser et al. reported that CYP17 gene expression increased for biosynthesis of androgens in theca interna cells in women with PCOS [17]. Moran et al. reported that women with PCOS who had an excess of adrenal androgen had significantly higher activity of CYP17 than that in women with PCOS who did not have an excess of adrenal androgen [16]. Thus, stimulation of DHEAS production by activation of CYP17A1 induces a hyperandrogenic state in women with PCOS [16, 17]. The results of those previous studies suggest that there are changes such as fibrosis in the ovarian stroma and transient increases in LH and androgens with aging. In Group C, production of androgen may have been started by the effect of increased LH level and a transition from the delta-4 pathway to the delta-5 pathway may have been proceeding. Negative correlations between FSH and estradiol were found to be significant in Group C and remarkable in Group D. When women enter into the periods of Group C and Group D, which indicate menopausal transition, the negative correlation between estradiol and FSH might become stronger due to the remarkable decline in estradiol level. As shown in Table 3, LH and FSH were negatively correlated with estradiol in Group D. In other words, estradiol levels decreased while levels LH and FSH increased in Group D, and we speculate that the site for production of steroid hormones may move from the ovary to the adrenal gland. Around the stage in Group D, changes in bone metabolism and lipid metabolism might be mainly involved in the decrease in estradiol level.
Murayama et al. reported that theca cells pretreated with a high concentration of LH showed increased CYP17 gene expression [18]. Oktem et al. reported that FSH up-regulated the mRNA expression of 17β-HSD and 3β-HSD in granulosa cells [19]. It has been reported that production of DHEAS is stimulated by an increase in LH in the adrenal gland in postmenopausal women [26]. In addition, production of DHEAS has been reported to be involved in CYP17A1 activity in the normal adrenal gland [27]. Due to an increase in LH in the late menopausal transition, we considered that CYP17A1 activity increases via LH receptors in the adrenal gland and the conversion from pregnenolone to DHEAS is stimulated. DHEAS level tended to increase, but the difference was not statistically significant (p = 0.062), in the present study. However, in a previous study, a transient increase in DHEAS was found in the late menopausal transition [28]. In the present study, LH was significantly associated with total T and free T in Group D (late menopausal transition). As well as DHEAS production in response to LH stimulation, conversion to T by stimulation of 17β-HSD activity via FSH increase is considered to be involved in this significant correlation [19]. The positive relationships between level of LH and levels of androgens including T, free T and DHEAS may indicate that the delta-5 pathway is the main pathway in Group D. In the late menopausal transition, LH and FSH may act cooperatively on enzyme activities and stimulate reproductive hormone production.
In Groups B, C, D and F, there were positive and significant associations between LH and FSH, but there was only a tendency for a correlation between LH and FSH in Group E. In the present study, in Group F, FSH level continued to increase, although LH level showed a plateau (Fig. 3). In groups B, C and D, both levels of LH and FSH increased in the same way. However, in group E, LH reached a plateau, but FSH continued to increase. Therefore, the time difference in hormonal levels in which a plateau was reached might be involved in the weak correlation between LH and FSH in Group E. The time difference in hormonal changes in which FSH reached a plateau later than LH might be involved in the weak correlation between LH and FSH in Group E. In addition, in Group E, the correlations of LH with T and free T shown in Group D disappeared. The reason may be the conversion from T to estradiol by an increase in aromatase through continuation of the increase in FSH, and this phenomenon was maintained in Group F.
Scatterplots of correlations of LH or FSH with reproductive hormones
In postmenopausal women, associations of FSH levels with the development of various diseases and with metabolism have been reported [29,30,31]. A high FSH level was shown to be associated with prevalence of vasomotor symptoms [32] and an increase in low-density lipoprotein cholesterol [5], and a low FSH level was shown to be associated with non-alcoholic fatty liver disease [33] and diabetes mellitus [29]. Serum FSH levels have been shown to be correlated with the rate of bone loss in perimenopausal women aged 42–52 years [34] and in postmenopausal women with a mean age of 81 years [35]. However, the associations that were investigated in those studies were for FSH levels, not LH levels, in postmenopausal women. The associations of FSH levels with lipid metabolism, carbohydrate metabolism and vascular function in postmenopause may be affected by the increase in androgen levels due to an increase in LH during the menopausal transition. Combined studies on LH levels and FSH levels from menopausal transition to postmenopause may be valuable.
Fibrosis in the stroma in the ovary and increases in LH and androstenedione occur in women with aging. Stimulation of 17β-HSD activity due to an increase in FSH might be regulated so as to prevent an excessive increase in androgen levels, particularly in postmenopausal women with high FSH levels. We did not examine the associations of LH and FSH with lipid metabolism and insulin resistance in each stage of the menopausal transition. Studies on associations of LH with the development of various diseases and with metabolism should be carried out not only for women in postmenopause but also for women during the menopausal transition.
There are some limitations in this study. The sample size in the present study might be insufficient for a generalization for all Japanese women. Further study with a large sample size is needed. This study was a cross-sectional study. Thus, a causal relationship needs to be clarified in a longitudinal study. In addition, measurements of various enzymes related to the production of hormones may be important to clarify individual differences in enzyme activities. In the present study, total circulating reproductive hormones were measured, and we could not separate ovary-derived reproductive hormones and adrenal gland-derived reproductive hormones.
The associations of LH and FSH with reproductive hormones are different depending on the stage of the menopausal transition.
All data and materials are available upon reasonable request from the corresponding author.
Sowers MR, Zheng H, McConnell D, Nan B, Harlow S, Randolph JF. Follicle stimulating hormone and its rate of change in defining menopause transition stages. J Clin Endocrinol Metab. 2008;93:3958–64. https://doi.org/10.1210/jc.2008-0482.
Article CAS PubMed PubMed Central Google Scholar
Tepper PG, Randolph JF, McConnell DS, Crawford SL, El Khoudary SR, Joffe H, Gold EB, Zheng H, Bromberger JT, Sutton-Tyrrell K. Trajectory clustering of estradiol and follicle-stimulating hormones during the menopausal transition among women in the study of women’s health across the nation (SWAN). J Clin Endocrinol Metab. 2012;97:2872–80. https://doi.org/10.1210/jc.2012-1422.
Article CAS PubMed PubMed Central Google Scholar
Sun L, Peng Y, Sharrow AC, Iqbal J, Zhang Z, Papachristou DJ, Zaidi S, Zhu LL, Yaroslavskiy BB, Zhou H, Zallone A, Sairam MR, Kumar TR, Bo W, Braun J, Cardoso-Landa L, Schaffler MB, Moonga BS, Blair HC, Zaidi M. FSH directly regulates bone mass.Cell.2006;247–60.https://doi.org/10.1016/j.cell.2006.01.051.
Robinson LJ, Tourkova I, Wang Y, Sharrow AC, Landau MS, Yaroslavskiy BB, Sun L, Zaidi M, Blair HC. FSH-receptor isoforms and FSH-dependent gene transcription in human monocytes and osteoclasts. Biochem Biophys Res Commun. 2010;26:12–7. Epub 2010 Feb 19.
Song Y, Wang ES, Xing LL, Shi S, Qu F, Zhang D, Li JY, Shu J, Meng Y, Sheng JZ, Zhou JH, Huang HF. Follicle-stimulating hormone induces postmenopausal dyslipidemia through inhibiting hepatic cholesterol metabolism. J Clin Endocrinol Metab. 2016;101:254–63. https://doi.org/10.1210/jc.2015-2724. Epub 2015 Nov 19.
Article CAS PubMed Google Scholar
Radu A, Pichon C, Camparo P, Antoine M, Allory Y, Couvelard A, Fromont G, Hai MT, Ghinea N. Expression of follicle-stimulating hormone receptor in tumor blood vessels. N Engl J Med. 2010;21:1621–30. https://doi.org/10.1056/NEJMoa1001283.
Serviente C, Tuomainen TP, Virtanen J, Witkowski S, Niskanen L, Bertone-Johnson.Follicle-stimulating hormone is associated with lipids in postmenopausal women.Menopause.2019;26:540–5.https://doi.org/10.1097/GME.0000000000001273.
Article PubMed PubMed Central Google Scholar
Sowers M, Zheng H, Tomey K, Karvonen-Gutierrez C, Jannausch M, Li X, Yosef M, Symons J. Changes in body composition in women over six years at midlife: ovarian and chronological aging. J Clin Endocrinol Metab. 2007;92:895–901. https://doi.org/10.1210/jc.2006-1393. Epub 2006 Dec 27.
Article CAS PubMed Google Scholar
Pabon JE, Li X, Lei ZM, Sanfilippo JS, Yussman MA, Rao CV. Novel presence of luteinizing hormone/chorionic gonadotropin receptors in human adrenal glands. J Clin Endocrinol Metab. 1996;81:2397–400.
Blair JA, Bhatta S, McGee H, Casadesus G. Luteinizing hormone: evidence for direct action in the CNS. Horm Behav. 2015;76:57–62. Epub 2015 Jul 12.
Article CAS PubMed PubMed Central Google Scholar
Pabon JE, Bird JS, Li X, Huang ZH, Lei ZM, Sanfilippo JS, Yussman MA, Rao CV. Human skin contains luteinizing hormone/chorionic gonadotropin receptors. J Clin Endocrinol Metab. 1996;81:2738–41. https://doi.org/10.1210/jcem.81.7.8675605.
Article CAS PubMed Google Scholar
Tao YX, Heit M, Lei ZM, Rao CV. The urinary bladder of a woman is a novel site of luteinizing hormone-human chorionic gonadotropin receptor gene expression. Am J Obstet Gynecol. 1998;179:1026–31. https://doi.org/10.1016/s0002-937898.
Article CAS PubMed Google Scholar
Alevizaki M, Saltiki K, Mantzou E, Anastasiou E, Huhtaniemi I. The adrenal gland may be a target of LH action in postmenopausal women.Eur J Endocrinol.2006;154:875–81.https://doi.org/10.1530/shaft.1.02165.
Article CAS PubMed Google Scholar
Santoro N, Torrens J, Crawford S, Allsworth JE, Finkelstein JS, Gold EB, Korenman S, Lasley WL, Luborsky JL, McConnell D, Sowers MF, Weiss G. Correlates of circulating androgens in mid-life women: the study of women’s Health across the Nation. J Clin Endocrinol Metab. 2005;90:4836–45. https://doi.org/10.1210/jc.2004-2063. Epub 2005 Apr 19.
Article CAS PubMed Google Scholar
Torrens JI, Sutton-Tyrrell K, Zhao X, Matthews K, Brockwell S, Sowers M, Santoro N. Relative androgen excess during the menopausal transition predicts incident metabolic syndrome in midlife women: study of women’s Health across the Nation. Menopause. 2009;16:257–64. https://doi.org/10.1097/gme.0b013e318185e249.
Article PubMed PubMed Central Google Scholar
Moran C, Reyna R, Boots LS, Azziz R. Adrenocortical hyperresponsiveness to corticotropin in polycystic ovary syndrome patients with adrenal androgen excess. Fertil Steril. 2004;81:126–31. https://doi.org/10.1016/j.fertnstert.2003.07.008.
Article CAS PubMed Google Scholar
Wickenheisser JK, Nelson-Degrave VL, McAllister JM. Dysregulation of cytochrome P450 17alpha-hydroxylase messenger ribonucleic acid stability in theca cells isolated from women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2005;90:1720–7. https://doi.org/10.1210/jc.2004-1860. Epub 2004 Dec 14.
Article CAS PubMed Google Scholar
Murayama C, Miyazaki H, Miyamoto A, Shimizu T. Luteinizing hormone (LH) regulates production of androstenedione and progesterone via control of histone acetylation of StAR and CYP17 promoters in ovarian theca cells. Mol Cell Endocrinol. 2012;5:1–9. Epub 2011 Dec 2.
Oktem O, Akin N, Bildik G, Yakin K, Alper E, Balaban B, Urman B. FSH Stimulation promotes progesterone synthesis and output from human granulosa cells without luteinization. Hum Reprod. 2017;32:643–52. https://doi.org/10.1093/humrep/dex010.
Article CAS PubMed Google Scholar
Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Reber RW, Sherman S, Sluss PM, de Villiers TJ, for the STRAW + 10 Collaborative Group. Executive summary of the stages of reproductive aging workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012;97:1159–68. https://doi.org/10.1210/jc.2011-3362. Epub 2012 Feb 16.
Article CAS PubMed PubMed Central Google Scholar
Kawakita T, Yasui T, Yoshida K, Matsui S, Iwasa T. Correlations of androstenediol with reproductive hormones and cortisol according to stages during the menopausal transition in japanese women. J Steroid Biochem Mol Biol. 2021;214:106009. https://doi.org/10.1016/j.jsbmb.2021.106009. Epub 2021 Sep 25.
Article CAS PubMed Google Scholar
Briley SM, Jasti S, McCracken JM, Hornick JE, Fegley B, Pritchard MT, Duncan FE. Reproductive age-associated fibrosis in the stroma of the mammalian ovary. Reproduction. 2016;152:245–60. https://doi.org/10.1530/REP-16-0129.
Article CAS PubMed PubMed Central Google Scholar
McCloskey CW, Cook DP, Kelly BS, Azzi F, Allen CH, Forsyth A, Upham J, Rayner KJ, Gray DA, Boyd RW, Murugkar S, Lo B, Trudel D, Senterman MK, Vanderhyden BC. Metformin abrogates age-associated ovarian fibrosis. Clin Cancer Res. 2020;26:632–42. https://doi.org/10.1158/1078-0432.CCR-19-0603.
Article CAS PubMed Google Scholar
Matt DW, Kauma SW, Pincus SM, Veldhuis JD, Evans WS. Characteristics of luteinizing hormone secretion in younger versus older premenopausal women. Am J Obstet Gynecol. 1998;178:504–10. https://doi.org/10.1016/s0002-9378(98)70429-6.
Article CAS PubMed Google Scholar
Schildkraut JM, Schwingl PJ, Bastos E, Evanoff A, Hughes C. Epithelial ovarian cancer risk among women with polycystic ovary syndrome. Obstet Gynecol. 1996;88:554–9. https://doi.org/10.1016/0029-7844(96)00226-8.
Article CAS PubMed Google Scholar
Alevizaki M, Saltiki K, Mantzou E, Anastasiou E, Huhtaniemi I. The adrenal gland may be a target of LH action in postmenopausal women.Eur J Endocrinol.2006 Jun;154(6):875–81.https://doi.org/10.1530/shaft.1.02165.
Richard J. Auchus Chap. 3G - genetic deficiencies of cytochrome P450c17 (CYP17A1): combined 17-Hydroxylase/17,20-Lyase Deficiency and isolated 17,20-Lyase Deficiency. Genetic Streroid Disorders. 2014;111–23. https://doi.org/10.1016/B978-0-12-416006-4.00009-0.
Matsui S, Yasui T, Tani A, Kato T, Kunimi K, Uemura H, Kuwahara A, Matsuzaki T, Irahara M. Association of circulating adiponectin with testosterone in women during the menopausal transition.Maturity.2012;73:255–60.https://doi.org/10.1016/j.maturity.2012.08.003.
Article CAS PubMed Google Scholar
Matthews KA, Chang Y, Brooks MM, Crawford SL, Janssen I, Joffe H, Kravitz HM, Thurston RC, El Khoudary SR. Identifying women who share patterns of reproductive hormones, vasomotor symptoms, and sleep maintenance problems across the menopause transition: group-based multi-trajectory modeling in the study of Women’s Health across the Nation. Menopause. 2020;5:126–34. https://doi.org/10.1097/GME.0000000000001663.
Chu MC, Rath KM, Huie J, Taylor HS. Elevated basal FSH in normal cycling women is associated with unfavourable lipid levels and increased cardiovascular risk. Hum Reprod. 2003;18:1570–3. https://doi.org/10.1093/humrep/deg330.
Article CAS PubMed Google Scholar
Wang N, Kuang L, Han B, Li Q, Chen Y, Zhu C, Chen Y, Xia F, Cang Z, Zhu C, Lu M, Meng Y, Guo H, Chen C, Lin D, Lu Y. Follicle- Stimulating hormone associates with prediabetes and diabetes in postmenopausal women. Acta Diabetol. 2016;53:227–36. https://doi.org/10.1007/s00592-015-0769-1. Epub 2015 May 12.
Article CAS PubMed Google Scholar
Randolph JF Jr, Sowers M, Bondarenko I, Gold EB, Greendale GA, Bromberger JT, Brockwell SE, Matthews KA. The relationship of longitudinal change in reproductive hormones and vasomotor symptoms during the menopausal transition. J Clin Endocrinol Metab. 2005;90:6106–12. https://doi.org/10.1210/jc.2005-1374. Epub 2005 Sep 6.
Article CAS PubMed Google Scholar
Wang N, Li Q, Han B, Chen Y, Zhu C, Chen Y, Xia F, Lu M, Meng Y, Guo Y, Ye L, Sui C, Kuang L, Lin D, Lu Y. Follicle-stimulating hormone is associated with non-alcoholic fatty liver disease in chinese women over 55 years old. J Gastroenterol Hepatol. 2016;31:1196–202. https://doi.org/10.1111/jgh.13271.
Article CAS PubMed Google Scholar
Sowers MR, Finkelstrein JS, Ettinger B, Bondarenko I, Neer RM, Cauley JA, Sherman S, Greendale GA, Study of Women’s Health Across the Nation. The association of endogenous hormone concentrations and bone mineral density measures in pre- and perimenopausal women of four ethnic groups: SWAN. Osteoporos Int. 2003;14:44–52. https://doi.org/10.1007/s00198-002-1307-x.
Article CAS PubMed Google Scholar
Veldhuis-Vlug AG, Woods GN, Sigurdsson S, Ewing SK, Le PT, Hue TF, Vittinghoff E, Xu K, Gudnason V, Sigurdsson G, Gift DM, Eiriksdottir G, Harris T, Schafer AL, Li X, Zaidi M, [ PubMed ] Rosen CJ, Schwartz AV.Serum FSH is associated with BMD, bone marrow adiposity, and body composition in the AGES-Reykjavik Study of Older Adults.J Clin Endocrinol Metab.2021;106:e1156–69.https://doi.org/10.1210/clinem/soil922.
We would like to express our deep gratitude to the subjects who participated in this study.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Department of Obstetrics and Gynecology, Institute of Biomedical Sciences, The University of Tokushima Graduate School, Tokushima, Japan
Takako Kawakita, Kanako Yoshida & Takeshi Iwasa
Department of Reproductive and Menopausal Medicine, Institute of Biomedical Sciences, The University of Tokushima Graduate School, Tokushima, Japan
Department of Obstetrics and Gynecology, Tokushima Red Cross Hospital, Tokushima, Japan
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
Takako Kawakita participated in research conception and design, data acquisition, data analysis and interpretation, drafting, and critical revision of the critical intellectual content. Toshiyuki Yasui participated in the conception and design of the study, data acquisition, data analysis and interpretation, and critical revision of the intellectual content of the paper. Kanako Yoshida participated in data analysis and interpretation, as well as critical revision of key intellectual content. Sumika Matsui participated in the conception and design of the study, data acquisition, data analysis and interpretation, and critical revision of the critical intellectual content. Takeshi Iwasa participated in data analysis and interpretation, as well as critical revision of key intellectual content. All authors reviewed the manuscript.
Informed consent was obtained from all participants before participating in the study. The study protocol was developed in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Tokushima University Hospital.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Kawakita, T., Yasui, T., Yoshida, K. et al. Associations of LH and FSH with reproductive hormones depending on each stage of the menopausal transition. BMC Women's Health 23, 286 (2023). https://doi.org/10.1186/s12905-023-02438-5
DOI: https://doi.org/10.1186/s12905-023-02438-5
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By using this website, you agree to our Terms and Conditions, Your US state privacy rights, Privacy statement and Cookies policy. Your privacy choices/Manage cookies we use in the preference centre.

Stimulate Spermatogenic Function © 2024 BioMed Central Ltd unless otherwise stated. Part of Springer Nature.